Column Finance and the Social Security System 2021.04.16
【Aging, safety net and fiscal crisis in Japan】No.302: Why has Japan, with the largest number of hospital beds in the world, not been able to secure beds for COVID-19 patients?
In this column series, Yukihiro Matsuyama, Research Director at CIGS introduces the latest information about aging, safety net and fiscal crisis in Japan with data of international comparison.
Why has Japan, with the largest number of hospital beds in the world, not been able to secure beds for COVID-19 patients?
According to OECD Health Statistics 2020, the number of beds per 1,000 people in 2017 was 13.05 in Japan, 8.0 in Germany, 5.98 in France, 2.87 in the United States, 2.54 in the United Kingdom, and 2.53 in Canada. From the outbreak of COVID-19 to April 2, 2021, the number of the infected per 1,000 people was 93.3 in the United States, 73.6 in France, 65.4 in the United Kingdom, 34.4 in Germany, and 26.3 in Canada, while it was 3.8 in Japan. Despite having a small number of COVID-19 patients and the largest number of beds in the world, Japan has a big political issue in that the beds for them are not sufficiently secured.
Table1. Number of hospitals and beds (as of December 31, 2020).
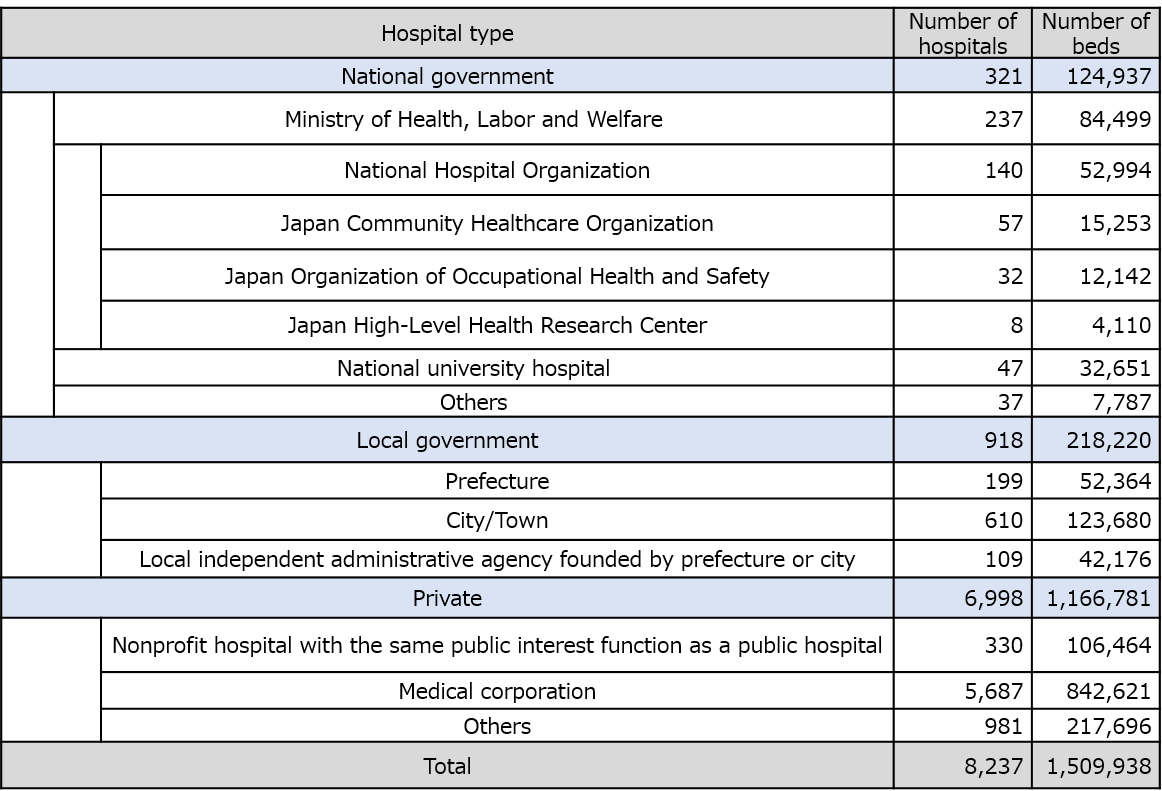
Source: Ministry of Health, Labor and Welfare
As shown in Table 1, the number of hospitals in Japan is 8,237, 5,687 of which are managed by medical corporations, accounting for 69%. Most medical corporations are for-profit enterprises that are private property, and their profits belong to the individual investors. The national government has provided a subsidy of JPY 19.5 million (US$ 177,000) per bed to encourage private hospitals to add new beds for COVID-19 patients. However, from January 2021 to March 2021, when the third-wave surge of the COVID-19 pandemic hit, the number of beds increased only 10.7%, from 27,515 to 30,450 (Figure 1), accounting for only 2% of the total number of beds of 1,509,938. Since the number of beds for critically ill COVID-19 patients is 4,248 compared to a total of 730 critically ill patients as of March 31, 2021, it seems that the medical care delivery system for COVID-19 is in place. However, not all of these beds can actually operate because of the difficulty in securing doctors and nurses to provide medical care to COVID-19 patients. The national government is asking medical institutions to double the number of COVID-19 beds to survive the already-begun fourth wave. In response to this request, medical organizations have argued that this is "difficult to achieve."
Figure 1. Number of beds for COVID-19 patients.
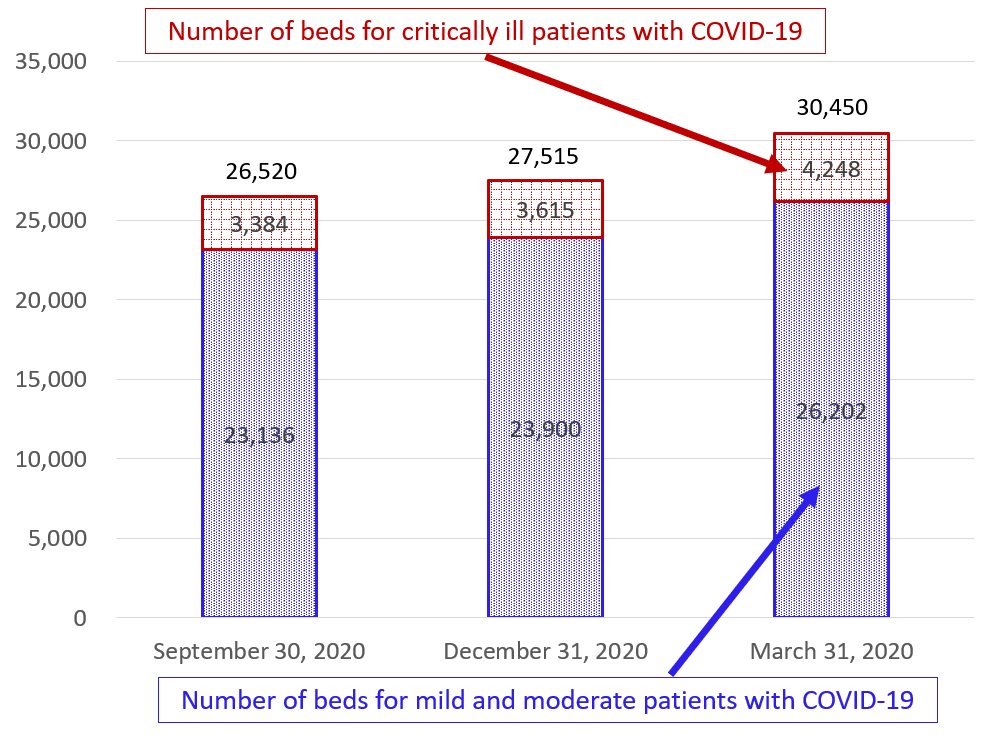
Source: Ministry of Health, Labor and Welfare
Currently, most COVID-19 beds are secured by national hospitals, public hospitals, nonprofit private hospitals, and national university hospitals. However, the structure of Japan's medical care delivery system for COVID-19 has major flaws that are not found overseas. A prerequisite for the system to avoid medical collapse during the COVID-19 pandemic is to separate it from regular medical care. Specifically, COVID-19 specialty hospitals that intensively accept COVID-19 patients should be established, and the regular medical patients of those hospitals need to be transferred to other hospitals. Such separation of COVID-19 medical care and regular medical care cannot be accomplished in one hospital. However, the Japanese government still adheres to the idea of installing COVID-19 beds in each hospital. As a result, as shown in Table 2, while 378 hospitals in Tokyo have stated that they will accept critically ill COVID-19 patients, 360 hospitals actually accept only 0 to 4 patients. These hospitals are hesitant to add COVID-19 beds due to the fear of nosocomial infections, in addition to the difficulty of securing human resources.
Table 2. Number of hospitals in Tokyo that have agreed to accept critically ill patients with COVID-19 versus the actual number admitted.
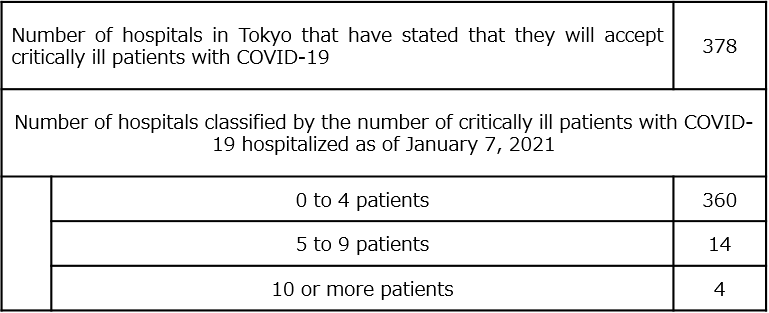
Note: A critically ill patient is defined as one who is hospitalized with ECMO/ventilator and ICU.
Source: Ministry of Health, Labor and Welfare
As shown in Table 1, the Ministry of Health, Labor and Welfare manages three general hospital groups: the National Hospital Organization, the Japan Community Healthcare Organization, and the Japan Organization of Occupational Health and Safety. However, each group consists of standalone hospitals scattered throughout the country, and there is no synergistic effect of integration through sharing of patient information as a whole group. Moreover, hospitals of the three groups that are in the same medical area compete with each other to get patients. National university hospitals also join in this harmful competition.
Overseas, the use of digital health is accelerating due to the COVID-19 pandemic. In Japan, however, none of these government-affiliated hospitals fulfill the platform function that forms the basis of digital health. As mentioned above, it is difficult to efficiently separate COVID-19 medical care and regular medical care within one hospital; thus, even if the government asks these hospitals to add more beds for COVID-19 patients, they do not work as expected. Even if the president of a hospital that ignores the request is fired, doctors and nurses do not always obey the government's orders as long as it is impossible to divide the functions within one hospital. This is because doctors and nurses can get a job at another hospital immediately after being dismissed.
In contrast to Japan, overseas medical entities such as the integrated healthcare networks (e.g., Kaiser Permanente) in the United States, Alberta Health Services in Canada, and the National Health Service in the United Kingdom have been established in peacetime as the last resort for each wide medical area. The keywords of these overseas medical entities are “integration” and “overall optimization.” At the outbreak of COVID-19, these entities set up COVID-19 specialty hospitals to clarify the division of roles with other facilities. As a result, they were able to maintain their medical care delivery systems despite an uncontrollable increase in patients with COVID-19. Therefore, the Japanese government should integrate hospitals of the National Hospital Organization, the Japan Community Health Care Organization, the Japan Organization of Occupational Health and Safety, and national universities in each wide medical area with a population of approximately 1 million. The total number of hospitals in these four groups is 276, and the total number of beds is 113,040. Therefore, it seems easy to secure the more than 20,000 additional beds needed for the fourth wave of the pandemic.
